Spondylolisthesis: Common Causes, Symptoms & Treatment Options. Speak To A Therapist Today. Call (24/7): 1300-003-777.
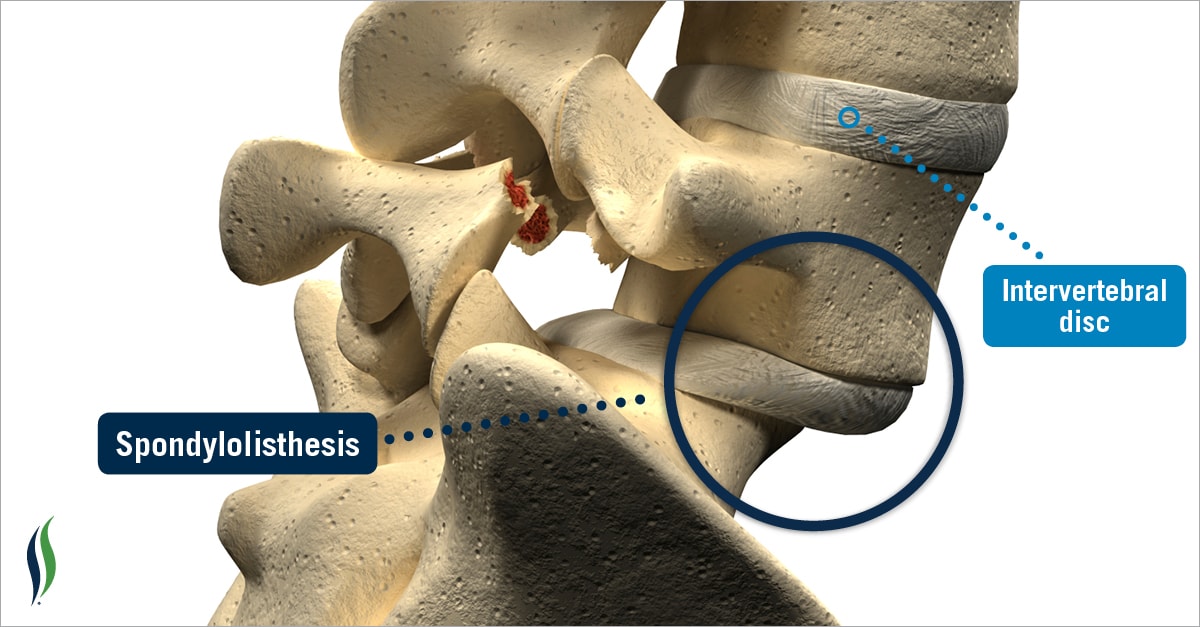
Spondylolisthesis occurs when a bone of the spine (referred to as a vertebra) moves or slips forward in relation to a vertebra above or below it. Spondylolisthesis usually affects lumbar spine vertebrae due to direct trauma, degenerative joint disease or a congenital abnormality. While Spondylolisthesis is relatively uncommon, many clients who present to our Chiropractic clinic suffering from it are unaware of their problem until further analysis and spinal imaging takes place. Discovering that you have Spondylolisthesis is extremely important because it influences the treatment which you’ll receive, your prognosis and therefore outcome.
Symptoms Of Spondylolysis
The hallmark symptoms of Spondylolisthesis will vary from person to persons, however commonly include:
- Generalized lower back pain that may refer to the buttock and legs.
- Chronic hamstring tightness or a sense that you have poor flexibility.
- Difficulty during particular lumbar spine ranges of motion (particularly extension or attempting to stand tall).
- An occasional clicking sensation of the lower back which may indicate instability.
- Numbness, lower limb muscle weakness and tingling may also be present.
Spondylolisthesis Causes
- Type 1 – Dysplastic/Congential Spondylolisthesis: The term congenital refers to an abnormality that is present from birth. This defect affects the articular process of the vertebra.
- Type 2 – Isthmic: Considered the most common form of Spondylolisthesis and is categorized into three sub-groups:
- Type 2(A): The result of repetitive micro-fractures of the pars interarticularis. Commonly seen in peope engaging in overuse type injuries.
- Type 2(B): Also the result of repetitive micro-fractures of the part interarticularis however the fracture is incomplete. The incomplete fracture may demonstrate healing and elongation leading to vertebra forward slippage.
- Type 2(C): Complete fracture is noted however is the result of a direct trauma or sustained injury.
- Type 3 – Degenerative: The spine and intervertebral discs lose elasticity and height as we age. A narrow spinal disc causes vertebrae to come into close contact. Eventually this process may lead to forward slippage.
- Type 4 – Fracture: Similar to other forms of Spondylolisthesis however the particular site of the fracture is different and may involve another aspect of the vertebra.
- Type 5 – Tumor: Tumors and other abnormalities may lead to bone weakening and therefore instability of joints.
- Type 6 – Surgical Intervention/Iatrogenic: Spinal surgery may lead to bone weakening such as a Laminectomy procedure.
Lumbopelvic Examination
- Subjective
- The subjective examination is one of most powerful tools a clinician can use. This involves a discussion about your presenting complaint to assist your practitioner in determining appropriate differential diagnoses which will guide their objective examination. Questions which you may expect to answer may include (but not limited too):
- What is your age?
- Can you remember how the injury or pain became apparent?
- How long have you been suffering with this pain?
- Are you able to pinpoint and locate the area of discomfort?
- Are you experiencing burning, tingling, numbness, weakness, shooting pain?
- Is the complaint improving, staying the same or worsening?
- Do you find any particular movements or actions difficult to perform?
- Do you note any difficulty going to the toilet?
- The subjective examination is one of most powerful tools a clinician can use. This involves a discussion about your presenting complaint to assist your practitioner in determining appropriate differential diagnoses which will guide their objective examination. Questions which you may expect to answer may include (but not limited too):
- Objective
- Your Chiropractor will observe your movement, range of motion, muscle strength, neurological function as well as performing various orthopaedic tests.
- Fear Avoidance Belief Questionnaire
- Acute Low Back Pain Screening Questionnaire
- The Quebec Back Pain Disability Scale
- Oswestry Disability Questionnaire (this outcome measure is considered the gold standard)
- Roland-Morris Disability Questionnaire
How Is It Diagnosed?
Diagnosis is heavily relied on X-ray images of the lower back. Lumbar spine X-rays will demonstrate which vertebra is effected as well as the degree of severity.
Spondylolisthesis Treatment
The main goal of managing Spondylolisthesis is to improve stability of the lumbar spine and associated core and gluteal muscles. Conservative care such as Chiropractic and Physiotherapy are shown to do well with mild (grade 1 to grade 2) slippages whereas for more severe cases medical referral is indicated.Chiropractic & Physiotherapy
Medical Referral
Chiropractor Spondylolisthesis Research
- A specifically tailored and individualized exercise regime concurrent with conservative management appears effective in managing symptoms associated with symptomatic Spondylolithesis. O’Sullivan, P. (1997). Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiological diagnosis of Spondylolysis or Spondylolithesis. Spine, 22(24); 2959 – 2967.
- Individuals suffering from severe degenerative Spondylolisthesis and spinal stenosis that were treated surgically demonstrated greater improvement then those non-surgically. Weinstein, J. (2007). Surgical versus non-surgical treatment for lumbar degenerative spondylolithesis. The New England Journal of Medicine.